A detailed examination of cutting-edge therapies and traditional approaches for managing canine OA pain.
78+ Sources
- Key Insights into Canine OA Management
- The Pathophysiology and Management Landscape of Canine Osteoarthritis
- Monoclonal Antibody Therapy: A Targeted Molecular Approach
- Homeopathic Formulations: The Case of Traumeel
- Comparative Analysis: Evidence, Efficacy, and Clinical Considerations
- Discussion and Implications for Veterinary Practice
- A Comprehensive Overview of Canine Osteoarthritis Treatment Approaches
- Video Deep Dive: Understanding Canine Arthritis
- Comparative Treatment Characteristics Table
- Frequently Asked Questions (FAQ)
- Conclusion
- Recommended Further Reading
- Referenced Search Results
Canine osteoarthritis (OA) represents a significant challenge in veterinary medicine, characterized by chronic pain, inflammation, and progressive joint degeneration that severely impacts a dog’s quality of life. As conventional treatments often come with limitations and potential side effects, the veterinary field continuously seeks more effective and safer alternatives. This comprehensive review delves into two distinct therapeutic avenues: monoclonal antibody (mAb) therapy, a targeted biological approach, and homeopathic treatments, which rely on highly diluted substances. By dissecting their underlying mechanisms, evaluating the robustness of their clinical evidence, and considering their practical implications, this analysis aims to provide clarity for veterinarians and pet owners navigating the complex landscape of canine OA management.
Key Insights into Canine OA Management
- Monoclonal Antibody Therapy (e.g., Bedinvetmab): Represents a significant scientific advancement, offering targeted pain relief by neutralizing nerve growth factor (NGF), a key pain mediator. Its efficacy and safety are supported by rigorous, large-scale clinical trials and regulatory approvals, establishing it as a primary treatment option.
- Homeopathic Treatments (e.g., Traumeel/Zeel): Operate on principles of extreme dilution with a largely unproven mechanism of action. While some limited, small-scale studies suggest minor benefits, the overall scientific consensus finds insufficient robust evidence to support their widespread efficacy beyond a potential placebo effect.
- Evidence-Based Decision Making: Veterinarians are encouraged to prioritize treatments with strong scientific backing, like monoclonal antibodies, and clearly communicate the differing levels of evidence for various therapies to pet owners, particularly regarding the potential for caregiver placebo with homeopathic approaches.
The Pathophysiology and Management Landscape of Canine Osteoarthritis
Osteoarthritis in dogs is a debilitating condition involving a complex interplay of mechanical stress, inflammation, and molecular changes within the joint. It is a leading cause of chronic pain, affecting a substantial percentage of the canine population, particularly as they age. Understanding its multifaceted nature is crucial for effective management.
The Molecular and Biomechanical Basis of Canine OA
At its core, OA is characterized by the degradation of articular cartilage, changes in the subchondral bone, and inflammation of the synovial membrane (synovitis). Key molecular mediators, such as cytokines (e.g., interleukin-1β, tumor necrosis factor-alpha), prostaglandins, and nerve growth factor (NGF), play critical roles in perpetuating pain signaling and cartilage destruction. Biomechanical factors, including genetic predisposition, conformation abnormalities, obesity, and previous joint injuries, can initiate or exacerbate the disease process. The elevation of NGF in osteoarthritic joints is particularly significant, as it contributes to both peripheral and central sensitization, leading to chronic pain and hyperalgesia.

Radiographic signs of joint disease in dogs and cats, illustrating the structural changes associated with OA.
Clinical Manifestations and Impact on Animal Welfare
The clinical signs of canine OA are varied and can range from subtle changes in behavior to overt lameness. Common manifestations include stiffness, reluctance to move, difficulty rising, decreased activity levels, altered gait, and hesitancy to jump or use stairs. Chronic pain and functional impairment can lead to significant reductions in a dog’s quality of life, often resulting in secondary behavioral changes such as irritability, lethargy, or aggression due to discomfort. Recognising these signs early is paramount for timely intervention and improving animal welfare.
Conventional Pharmaceutical Interventions and Their Limitations
Traditionally, non-steroidal anti-inflammatory drugs (NSAIDs) have been the cornerstone of pharmaceutical management for canine OA due to their analgesic and anti-inflammatory properties. While highly effective in many cases, long-term use of NSAIDs can be associated with adverse effects, including gastrointestinal upset, renal toxicity, and hepatic issues. These limitations, along with instances of inadequate response or contraindications in certain patients, have fueled the search for alternative and more targeted therapeutic options that offer effective pain management with improved safety profiles.
Monoclonal Antibody Therapy: A Targeted Molecular Approach
Monoclonal antibody therapy represents a significant leap forward in veterinary medicine, offering a highly targeted and effective solution for managing canine OA pain. This innovative approach harnesses the power of specific antibodies to neutralize key mediators of pain and inflammation.
Mechanism of Action: Neutralizing Key Pain and Inflammation Mediators
At the forefront of monoclonal antibody therapy for canine OA is bedinvetmab, marketed as Librela. Bedinvetmab is a fully canine anti-nerve growth factor (NGF) monoclonal antibody. NGF is a crucial protein involved in pain signaling, and its levels are elevated in osteoarthritic joints, contributing significantly to chronic pain. Bedinvetmab works by specifically binding to and sequestering NGF, thereby preventing it from interacting with its receptors (TrkA and p75). This action effectively blocks the transmission of pain signals, reduces neurogenic inflammation, and desensitizes nociceptors, leading to sustained analgesia without the systemic effects often associated with NSAIDs. A key advantage of this mechanism is its minimal involvement with the liver or kidneys, making it a viable option for dogs with co-existing conditions that might contraindicate other pain medications.

A visual representation of monoclonal antibodies specifically designed to target and neutralize disease-causing molecules.
Clinical Evidence for Efficacy and Safety in Canine OA
The efficacy and safety of bedinvetmab are well-supported by robust clinical evidence, including prospective, randomized, double-blind, placebo-controlled multisite studies. These gold-standard trials have consistently demonstrated significant improvements in pain severity, pain interference with daily activities, and overall quality of life in dogs with OA. For instance, studies have shown that dogs receiving monthly bedinvetmab injections experienced substantial reductions in pain scores, with responses maintained over extended periods, often up to nine months. The FDA’s approval of bedinvetmab (Librela) in 2023 for the control of pain associated with canine OA underscores its proven efficacy and favorable safety profile, marking it as the first monoclonal antibody approved for this use in dogs. Comparative data also suggest that bedinvetmab can provide pain management comparable to or even superior to some traditional NSAIDs.
Pharmacovigilance and Real-World Application (e.g., Bedinvetmab)
Post-approval pharmacovigilance and real-world data continue to affirm the positive impact of bedinvetmab. Veterinarians report high satisfaction with its effectiveness, with ratings often around 8.6 out of 10 for OA pain management. While generally considered safe, ongoing monitoring allows for the identification of any potential long-term or rare adverse events. The unique mechanism of action of monoclonal antibodies makes them less likely to cause gastrointestinal side effects compared to NSAIDs, broadening their applicability, especially for dogs where NSAID use is limited. This consistent positive feedback from real-world application, combined with its strong scientific foundation, positions bedinvetmab as a pivotal advancement in canine OA pain control.
Homeopathic Formulations: The Case of Traumeel
Homeopathic treatments represent a fundamentally different approach to disease management, with principles that diverge sharply from conventional medicine. While popular among some pet owners seeking “natural” remedies, their scientific basis and clinical efficacy for conditions like canine OA are subjects of considerable debate.
Principles of Homeopathy in Veterinary Medicine
Homeopathy operates on the principle of “like cures like” (similia similibus curentur), meaning a substance that causes symptoms in a healthy individual can, in highly diluted forms, treat similar symptoms in a sick individual. Homeopathic remedies are prepared through a process of serial dilution and succussion (vigorous shaking), often to the point where the original substance is theoretically no longer present in the final product. Proponents believe these highly diluted substances stimulate the body’s self-healing mechanisms. In veterinary practice, homeopathic remedies like Traumeel or Zeel (a similar homeopathic combination preparation) are sometimes used for pain and inflammation, including those associated with OA.
A Critical Review of Clinical Studies on Traumeel for Pain Management
Clinical studies evaluating the efficacy of homeopathic formulations for canine OA, such as Traumeel or Zeel, are notably scarce and often suffer from significant methodological limitations. While a few small, older studies have suggested modest short-term pain relief in dogs with OA, these findings are not consistently replicated in more robust research. For example, one study on Zeel indicated some pain reduction compared to a placebo group, but it also noted that its efficacy was not comparable to established conventional treatments like carprofen. The lack of large-scale, well-designed, randomized, placebo-controlled trials makes it challenging to draw definitive conclusions about their true therapeutic effects.
Analysis of Placebo-Controlled Trials and Methodological Challenges
A major challenge in assessing homeopathic treatments is distinguishing any true physiological effect from the placebo effect. Many studies on homeopathy, particularly in veterinary medicine, lack rigorous blinding and adequate control groups, making them susceptible to bias, including the “caregiver placebo phenomenon.” This phenomenon occurs when an owner’s belief in a treatment influences their perception of their pet’s improvement, even if the treatment itself has no direct biological effect. Scientific reviews generally conclude that there is insufficient robust evidence to support the efficacy of homeopathic treatments for canine OA beyond that of a placebo. The ultra-high dilutions used in homeopathy also present a challenge to establishing a plausible biological mechanism of action, leading to widespread skepticism within the scientific community.
Comparative Analysis: Evidence, Efficacy, and Clinical Considerations
A direct comparison between monoclonal antibody therapy and homeopathic treatments for canine OA reveals stark differences in their scientific foundations, mechanisms, and the strength of their evidence bases. Understanding these distinctions is critical for informed veterinary decision-making.
Head-to-Head Comparison of Mechanisms: Targeted Biology vs. Homeopathic Dilution
Monoclonal antibodies operate on a clear, scientifically understood biological principle: they are engineered proteins designed to specifically bind to and neutralize a target molecule, like NGF, that is known to play a direct role in the disease pathology. This represents a highly targeted and evidence-based approach to pain management, directly interfering with a validated physiological pathway. In contrast, homeopathic formulations rely on principles of extreme dilution, often beyond Avogadro’s number, implying that no original molecules of the active substance remain. The proposed mechanism of action, often vaguely described as stimulating the body’s vital force or natural healing processes, lacks any plausible biological explanation consistent with current scientific understanding. This fundamental difference in mechanistic plausibility is a core point of divergence.
Evaluating the Strength of the Evidence Base: Clinical Trials vs. Anecdotal Reports
The evidence supporting monoclonal antibody therapy is built upon a foundation of rigorous, large-scale, prospective, randomized, double-blind, placebo-controlled clinical trials—the gold standard for evaluating medical interventions. These trials demonstrate statistically significant and clinically meaningful improvements in pain and quality of life, leading to regulatory approvals from bodies like the FDA. The data are transparent, replicable, and withstand scientific scrutiny. Conversely, the evidence for homeopathic treatments is largely characterized by anecdotal reports, small-scale studies with significant methodological flaws (e.g., lack of blinding, inadequate controls, small sample sizes), and inconsistent results. Systematic reviews and major scientific organizations consistently conclude that there is a lack of robust, independent, high-quality evidence to support the efficacy of homeopathy beyond a placebo effect. This disparity in the strength and quality of evidence is perhaps the most critical distinguishing factor.
The Role of the Placebo Effect and the Caregiver Placebo Phenomenon
The placebo effect is a well-documented phenomenon where a perceived improvement occurs due to the patient’s (or, in veterinary medicine, the owner’s) belief in the treatment, rather than any direct pharmacological action. In canine OA, this often manifests as the “caregiver placebo phenomenon,” where an owner’s hope and expectation for a homeopathic remedy can influence their subjective assessment of their dog’s pain and mobility. While the placebo effect can be beneficial, it does not represent a true therapeutic effect of the substance itself. High-quality clinical trials for monoclonal antibodies are specifically designed to mitigate the influence of the placebo effect through rigorous blinding and controlled comparisons, ensuring that observed improvements are attributable to the drug. Homeopathic studies, particularly those relying on subjective owner-reported outcomes without robust controls, are highly susceptible to the caregiver placebo phenomenon, making it difficult to ascertain any genuine efficacy.
The following radar chart visually compares the perceived scientific robustness, clinical evidence, and mechanistic plausibility of monoclonal antibody therapy against homeopathic treatments for canine osteoarthritis. This chart reflects the consensus derived from rigorous scientific reviews and clinical trial data.
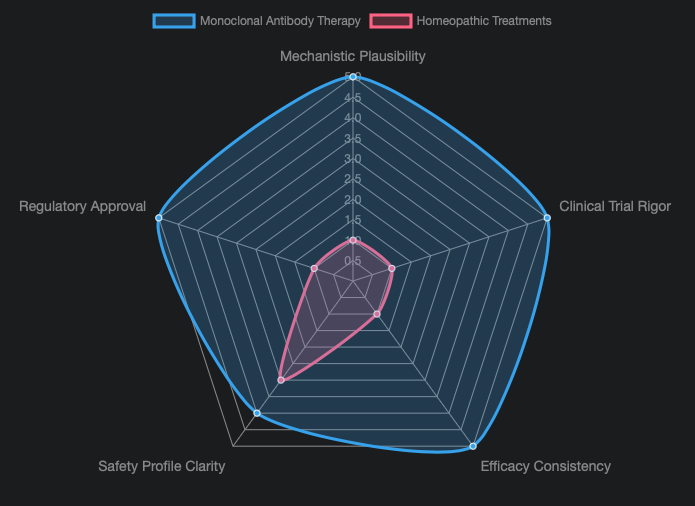
This radar chart clearly illustrates the significant differences in scientific support between the two approaches. Monoclonal antibody therapy consistently scores high across all parameters, reflecting its strong foundation in evidence-based medicine. Conversely, homeopathic treatments demonstrate very low scores, particularly in mechanistic plausibility, clinical trial rigor, efficacy consistency, and regulatory approval, aligning with the scientific consensus that their benefits are largely unsubstantiated.
Discussion and Implications for Veterinary Practice
Navigating the diverse range of treatment options for canine OA requires an evidence-based approach and clear communication with pet owners. This section synthesizes the implications of the comparative analysis for practical veterinary application.
Formulating an Evidence-Based Treatment Hierarchy
Based on the overwhelming evidence, monoclonal antibody therapy (such as bedinvetmab) should be prioritized as a first-line treatment for OA pain in dogs, alongside or as an alternative to NSAIDs, especially in cases where NSAIDs are contraindicated or less effective. A comprehensive OA management plan should ideally be multimodal, incorporating several strategies to address different aspects of the disease. This evidence-based hierarchy typically includes:
Core Management Strategies:
- Weight Optimization: Reducing excess weight significantly lessens the load on affected joints.
- Controlled Exercise and Physiotherapy: Tailored exercise programs, hydrotherapy, and manual therapies help maintain muscle mass, joint flexibility, and overall mobility.
- Environmental Modification: Providing comfortable bedding, ramps, and non-slip surfaces can improve mobility and reduce strain.
- Nutraceuticals: Omega-3 fatty acids and green-lipped mussel supplements, while not providing immediate pain relief, can offer anti-inflammatory benefits and support joint health over time.
First-Line Analgesia:
- NSAIDs: Remain a primary choice for managing pain and inflammation.
- Anti-NGF Monoclonal Antibodies: Offer a targeted approach, particularly valuable for long-term management and in patients with NSAID sensitivities.
Adjunctive Therapies:
- Gabapentin and Amantadine: Can be used as adjuncts for neuropathic pain or central sensitization in more severe cases.
- Injectable Polysulfated Glycosaminoglycans (PSGAGs): Support cartilage health and reduce inflammation.
- Intra-articular Therapies: Such as corticosteroids, hyaluronic acid, or platelet-rich plasma (PRP), can provide localized relief.
- Stem Cell Therapy: An emerging option for some cases.
Homeopathic products, due to the lack of robust scientific evidence, should not be recommended as primary or even adjunctive analgesics for canine OA. Their use risks delaying effective, evidence-based care.

A dog undergoing physical therapy for osteoarthritis, emphasizing the importance of multimodal treatment strategies.
Communicating Treatment Options and Evidence to Pet Owners
Effective communication is paramount. Veterinarians have a responsibility to educate pet owners about the various treatment options, their expected benefits, potential risks, and critically, the strength of the scientific evidence supporting each. When discussing monoclonal antibodies, it’s important to explain their targeted mechanism, proven efficacy, safety profile, and convenience of monthly injections. For homeopathic treatments, it is crucial to clearly state the limited and often low-quality evidence, the lack of a plausible mechanism, and the significant role of the caregiver placebo phenomenon. Explaining that pursuing unproven therapies might delay access to genuinely effective treatments is also vital. This transparency empowers owners to make informed decisions that are truly in the best interest of their pets’ health and welfare.
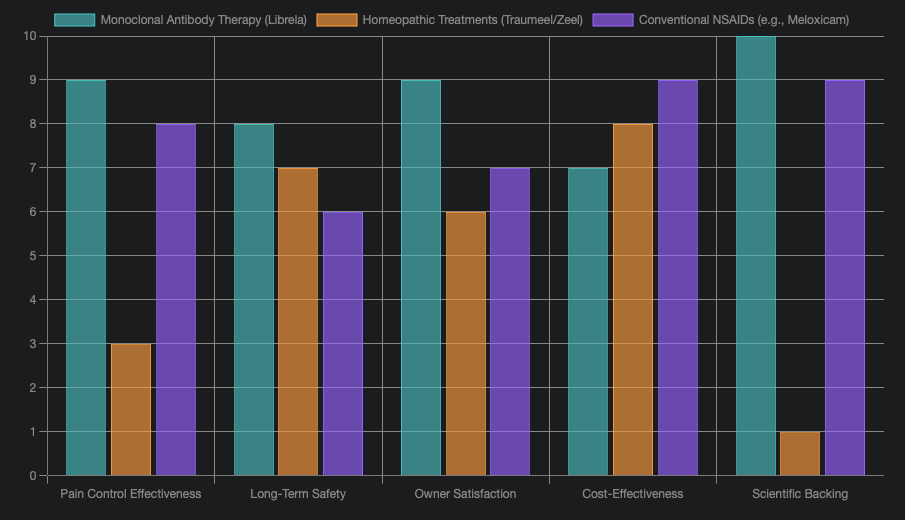
The bar chart above provides a comparative assessment of monoclonal antibody therapy, homeopathic treatments, and conventional NSAIDs across various practical considerations for canine OA management. While homeopathic treatments might appear cost-effective initially and have lower direct side effects, their significant lack of scientific backing and lower perceived efficacy make them a less reliable option for veterinarians seeking predictable and evidence-based outcomes. Monoclonal antibodies and NSAIDs demonstrate strong profiles in pain control and scientific support, with varying degrees of long-term safety and owner satisfaction.
Future Research Directions in Canine Arthritis Management
The field of canine OA management is continually evolving. Future research should focus on:
- Optimizing Monoclonal Antibody Therapies: This includes head-to-head comparisons of bedinvetmab with traditional NSAIDs using objective biomechanical endpoints, as well as investigating the safety and efficacy of combination therapies (e.g., mAb plus NSAID).
- Exploring Novel Biologics: Continued development of other anti-NGF mAbs and injectable compounds, potentially with disease-modifying properties.
- Advanced Diagnostics: Improving early OA detection guided by consensus staging frameworks (e.g., COAST).
- High-Quality Homeopathy Studies: While skepticism remains, if homeopathic treatments are to be considered, they require rigorous, adequately powered, blinded, placebo-controlled trials to unequivocally demonstrate any efficacy beyond placebo.
A Comprehensive Overview of Canine Osteoarthritis Treatment Approaches
This mindmap visually summarizes the diverse approaches to managing canine osteoarthritis, categorizing them by their scientific foundation and application.
mindmap
root[“Canine Osteoarthritis Management”]
Monoclonal_Antibody_Therapy[“Monoclonal Antibody Therapy (e.g., Bedinvetmab)”]
Targeted_Mechanism[“Targeted Mechanism: Anti-NGF”]
Robust_Evidence[“Robust Evidence: Clinical Trials, FDA Approval”]
High_Efficacy[“High Efficacy: Pain Relief, QoL Improvement”]
Favorable_Safety[“Favorable Safety Profile: Minimal Organ Involvement”]
Monthly_Injection[“Monthly Injection”]
Homeopathic_Treatments[“Homeopathic Treatments (e.g., Traumeel/Zeel)”]
Dilution_Principle[“Principle: Extreme Dilution (#quot;Like Cures Like#quot;)”]
Limited_Evidence[“Limited/Inconsistent Evidence: Small, Flawed Studies”]
Unproven_Mechanism[“Unproven Mechanism of Action”]
Placebo_Effect_Risk[“High Risk of Placebo Effect / Caregiver Placebo”]
Not_Recommended_Primary[“Not Recommended as Primary Therapy”]
Conventional_Pharmaceuticals[“Conventional Pharmaceuticals”]
NSAIDs_Pharma[“NSAIDs (e.g., Meloxicam, Carprofen)”]
Pain_Inflammation_Relief[“Pain & Inflammation Relief”]
Potential_Side_Effects[“Potential GI/Renal/Hepatic Side Effects”]
Adjunctive_Meds[“Adjunctive Medications (e.g., Gabapentin, Amantadine)”]
Neuropathic_Pain[“Addresses Neuropathic Pain”]
Non_Pharmaceutical_Approaches[“Non-Pharmaceutical Approaches”]
Weight_Management[“Weight Management”]
Physical_Therapy[“Physical Therapy (Hydrotherapy, Exercises)”]
Nutraceuticals[“Nutraceuticals (Omega-3s, GLM)”]
Environmental_Modifications[“Environmental Modifications”]
Emerging_Therapies[“Emerging Therapies”]
Stem_Cell_Therapy[“Stem Cell Therapy”]
PRP_Injections[“PRP Injections”]
New_Biologics[“Other New Biologics”]
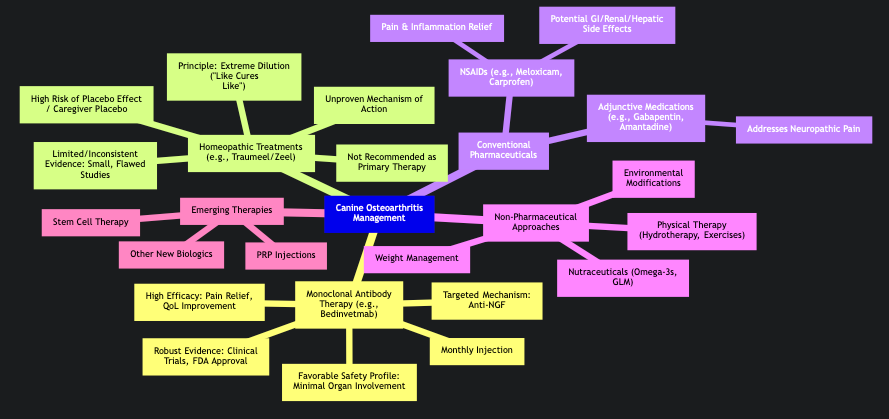
This mindmap provides a clear visual hierarchy of treatment options, emphasizing the distinct characteristics and evidentiary support for each approach, from the scientifically validated monoclonal antibodies to the less substantiated homeopathic remedies.
Video Deep Dive: Understanding Canine Arthritis
To further contextualize the discussion around canine osteoarthritis and its various treatments, the following video offers a valuable overview of the condition and how it affects our canine companions. It covers symptoms, diagnosis, and general management strategies, providing a broader understanding of the challenges pet owners and veterinarians face.
A comprehensive overview of canine arthritis, its symptoms, and general management strategies by a veterinarian.
This video titled “Pet Arthritis & Pain Management | Vet Tips” provides an excellent foundation for understanding canine osteoarthritis. It explains how arthritis commonly affects dogs and cats, particularly as they age, leading to pain and reduced mobility. The veterinarian in the video discusses the various signs owners should look out for, which can often be subtle, and the importance of early diagnosis. While it doesn’t delve specifically into monoclonal antibodies or homeopathy, it broadly covers traditional pain management techniques, physical therapy, and lifestyle adjustments that are part of a multimodal approach to OA care. This context is crucial because it highlights the universal goal of improving the quality of life for arthritic pets, regardless of the specific treatment chosen. It underscores that any effective therapy must address the core issue of pain and its impact on a dog’s daily activities, a benchmark against which all treatments, including new biologics and traditional remedies, must be measured.
Comparative Treatment Characteristics Table
This table offers a direct comparison of key characteristics for Monoclonal Antibody Therapy, Homeopathic Treatments, and Conventional NSAIDs in the context of canine osteoarthritis management.
| Feature | Monoclonal Antibody Therapy (e.g., Bedinvetmab) | Homeopathic Treatments (e.g., Traumeel/Zeel) | Conventional NSAIDs (e.g., Meloxicam) |
|---|---|---|---|
| Mechanism of Action | Highly targeted, neutralizes specific pain mediator (NGF) | Based on extreme dilutions; mechanism unproven/controversial | Reduces inflammation and pain by inhibiting prostaglandin synthesis (COX) |
| Strength of Evidence | Robust (large, blinded, placebo-controlled trials; FDA approved) | Weak (anecdotal, small, flawed studies; not widely supported) | Strong (extensive clinical trials; regulatory approved) |
| Efficacy | High, sustained pain relief and improved quality of life | Limited to no proven efficacy beyond placebo effect | High, effective for pain and inflammation |
| Safety Profile | Favorable, minimal systemic side effects (no liver/kidney metabolism) | Generally considered safe due to extreme dilution, but may delay effective treatment | Potential for gastrointestinal, renal, hepatic side effects with long-term use |
| Route of Administration | Monthly subcutaneous injection | Oral (drops, pellets) or topical application | Oral (daily), sometimes injectable |
| Regulatory Status (for OA) | Approved (e.g., FDA, EMA) | Not approved for specific OA indications based on efficacy | Approved |
| Suitability for Co-morbidities | Excellent, especially for dogs with organ sensitivities (e.g., renal disease) | No specific contraindications, but efficacy concerns remain | Caution with pre-existing kidney/liver disease, GI issues |
Frequently Asked Questions (FAQ)
What is canine osteoarthritis (OA)?
Canine osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, inflammation, and chronic pain, significantly impacting a dog’s mobility and quality of life.
How do monoclonal antibodies treat canine OA?
Monoclonal antibodies, like bedinvetmab (Librela), target and neutralize nerve growth factor (NGF), a protein that plays a key role in pain signaling in osteoarthritic joints, thereby reducing pain and inflammation.
Are homeopathic treatments effective for canine OA?
Based on current scientific evidence, there is insufficient robust data to support the efficacy of homeopathic treatments for canine OA beyond a potential placebo effect. Many studies are small and methodologically flawed.
What is the “caregiver placebo phenomenon”?
The “caregiver placebo phenomenon” in veterinary medicine refers to situations where a pet owner’s belief in a treatment influences their perception of their pet’s improvement, even if the treatment itself has no direct biological effect. This can complicate the assessment of treatments like homeopathy.
Can monoclonal antibodies be used with other OA treatments?
Yes, monoclonal antibodies are often part of a multimodal treatment plan for OA, which may include weight management, physical therapy, and other adjunctive medications as determined by a veterinarian.
Conclusion
The comparative analysis of monoclonal antibody therapy and homeopathic treatments for canine osteoarthritis highlights a clear distinction in their scientific validity and clinical utility. Monoclonal antibody therapy, exemplified by bedinvetmab, represents a significant, evidence-based advancement in pain management for canine OA. Its targeted mechanism of action, supported by rigorous clinical trials and regulatory approvals, provides consistent and effective pain relief with a favorable safety profile, making it a strong primary recommendation for veterinarians. In stark contrast, homeopathic treatments, while appealing to some for their “natural” perception, lack credible scientific evidence of efficacy beyond a potential placebo effect. Their mechanisms are unproven, and studies supporting their use are often methodologically weak and inconsistent. Therefore, an evidence-based approach to canine OA management prioritizes treatments with validated efficacy, such as monoclonal antibodies and conventional NSAIDs, integrating them into a comprehensive multimodal plan that also includes lifestyle modifications and supportive therapies. Clear and transparent communication with pet owners about the scientific merits and limitations of all available options is paramount to ensure the best possible outcomes for dogs suffering from osteoarthritis.
Recommended Further Reading
- Understanding the Mechanism of Action of Anti-NGF Monoclonal Antibodies in Canine Pain
- Evidence-Based Multimodal Approach to Canine Osteoarthritis Management
- The Role of Placebo Effect in Veterinary Medicine and Pain Perception
- Advances in Targeted Biologics for Chronic Pain in Dogs
Referenced Search Results
frontiersin.org
fda.gov
FDA Approves First Monoclonal Antibody for Dogs with Osteoarthritis Pain. – FDA
veterinaryevidence.org
sciencedirect.com
frontiersin.org
vet.cornell.edu
vethelpdirect.com
Monoclonal antibodies: The new treatments for arthritis in dogs and cats. – Vet Help Direct
vethelpdirect.com
Homeopathy for dogs and cats – what’s the evidence? – Vet Help Direct
pmc.ncbi.nlm.nih.gov
Evaluating Complementary Therapies for Canine Osteoarthritis—Part …
covalx.com
Humanized, Mouse or Chimeric Anti-CD47 Monoclonal Antibodies – CovalX
journals.plos.org
Enflicoxib for canine osteoarthritis: A randomized, blind, multicentre …
stemcellvet.co.uk
Homoeopathic Remedies For Arthritis In Dogs – Stem Cell Vet – …
avma.org
A closer look at veterinary homeopathy
amazon.com
Amazon.com: MediNatura T-Relief Pet Arthritis Relief Arnica +12 …
reddit.com
Homeopathic (aka Nosodes) vaccinations vs traditional … – Reddit
peopleforanimalsindia.org
zumalka.com
A Surprising Vet-Approved Home Remedy for Dog Arthritis That Really …
mdpi.com
A 2022 Systematic Review and Meta-Analysis of Enriched … – MDPI
mckeevervetderm.com
Microsoft Word – Monoclonal Antibody Therapy for Allergies in Dogs.docx
dogsnaturallymagazine.com
Top 5 Remedies For Dog Joint Pain And Injury – Dogs Naturally
news.zoetis.com
vitalanimal.com
Case Report: Rattlesnake Bite Cured with Homeopathy
pivh.org
Homeopathic Treatment for Immune-Mediated Polyarthritis, by Sarah …
eastcoastvet.com
Librela vs Adequan: Effective Treatments for Osteoarthritis …
veterinarypartner.vin.com
Medications for Degenerative Arthritis in Dogs and Cats
covalx.com
Caninized Human Antibodies To Human and Canine IL-4R Alpha – CovalX
schnauzer-forum.co.uk
Increased immunity using homeopathic canine nosodes
vetmed.illinois.edu
What Monoclonal Antibodies Can Do for Your Pet – Veterinary Medicine at Illinois
pmc.ncbi.nlm.nih.gov
covalx.com
Humanized, Mouse or Chimeric Anti-CD47 Monoclonal Antibodies – CovalX
trupanion.com
What is Homeopathy for Pets? Efficacy, Safety & Treatment
pagepress.org
Canine osteoarthritis and treatments: a review | Veterinary Science …
dogsnaturallymagazine.com
Cytopoint For Dogs: Is It Really Safe?
goelvetpharma.com
Homeopathy for Osteoarthritis in Dogs: Natural Pain Relief – …
todaysveterinarypractice.com
Select Drugs and Compounds for Canine Osteoarthritis …
vaajournal.org
pubmed.ncbi.nlm.nih.gov
1800petmeds.com
Joint Pain: How Holistic and Homeopathic Remedies Can Help Your …
saiba-animalhealth.com
Pet medicine in the modern age
dvm360.com
FDA approves first monoclonal antibody for managing OA pain in dogs
pmc.ncbi.nlm.nih.gov
Advances in the pharmaceutical treatment options for canine …
shirleys-wellness-cafe.com
I Cured My Sick Dog With Natural Home Remedies
pmc.ncbi.nlm.nih.gov
Therapeutic evaluation of homeopathic treatment for canine oral …
avma.org
Monoclonal antibodies show promise as new therapy for veterinary patients
bestfriends.org
Cat and Dog Arthritis Treatment | Best Friends Animal Society
zoetisus.com
Librela™ (bedinvetmab injection) For use with Canine
onlinelibrary.wiley.com
Current evidence for non‐pharmaceutical, non‐surgical treatments …
crossroads.pet
Understanding the difference between canine arthritis …
zoetisus.com
New Insights Into Canine And Feline OA Pain
avma.org
pmc.ncbi.nlm.nih.gov
Current Review of Monoclonal Antibody Therapeutics in Small …
quora.com
What is the best homeopathic remedy for my dog’s arthritis? The vet …
covalx.com
covalx.com
Antibodies Against Canine PD-1 – CovalX
pmc.ncbi.nlm.nih.gov
A pilot study examining a proprietary herbal blend for the treatment …
covalx.com
Antibodies to Canine Interleukin-4 Receptor Alpha – CovalX
charlesloopsdvm.com
Charles Loops, DVM – Arthritis Remedies
onlinelibrary.wiley.com
Evaluating Complementary Therapies for Canine Osteoarthritis …
timesonline.com
Dr. Maro: Monoclonal antibodies/biologicals for pets: New medications for old problems
zoetisus.com
Librela a new era in treatment | For Animal Healthcare Professionals
npr.org
Pets Deserve Evidence-Based Medicine, Too, Says The SkeptVet
fiercepharma.com
Aratana scores a ‘first’ with USDA approval for canine lymphoma drug | Fierce Pharma
pmc.ncbi.nlm.nih.gov
Treatment of canine osteoarthritis with allogeneic platelet …
mybiosource.com
Shop & Learn about Monoclonal Antibodies – MyBioSource
caninearthritis.org
Librela: What we know and don’t know | Canine Arthritis Resources and Education
fiercepharma.com
Aratana shares soar on first FDA approval of canine arthritis drug | Fierce Pharma
dogsnaturallymagazine.com
Librela (Beransa) – Wonder Drug Or Disaster In The Making?
frontiersin.org
COAST Development Group’s international consensus …
petmd.com
5 Tips for Treating and Beating Canine Lymphoma – PetMD
pivh.org
researchgate.net
A Homeopathic Combination Preparation (Zeel®) – ResearchGate
covalx.com
Humanized, Mouse or Chimeric Anti-CD47 Monoclonal Antibodies – CovalX
akc.org
Librela for Dogs: Uses, Side Effects, and Alternatives
pubmed.ncbi.nlm.nih.gov
shirleys-wellness-cafe.com
Saving My Dog’s Life With Home Care and Nutrition!
pubmed.ncbi.nlm.nih.gov
riney.vet.cornell.edu
Monoclonal Antibodies – March 2024
avmajournals.avma.org
Nutrition and nutraceuticals in the changing management of …
Last updated September 9, 2025