In an environment of heightened public concern over the rising prevalence of Autism Spectrum Disorder (ASD), the dissemination of accurate, evidence-based information by public health authorities is paramount. This article provides a critical medical and scientific review of a series of claims regarding the etiology of autism, allegedly put forth by the Department of Health and Human Services (HHS). These claims—ranging from the role of prenatal medication use to the influence of vaccination and diagnostic practices—diverge significantly from the established scientific consensus. This analysis will systematically deconstruct each assertion, juxtaposing it with current epidemiological and clinical evidence. Furthermore, it will elucidate the scientifically recognized factors contributing to the observed increase in ASD prevalence and conclude with evidence-based recommendations for public health policy, clinical practice, and future research.
1. Deconstructing Claims on Prenatal Exposures and Nutritional Deficiencies
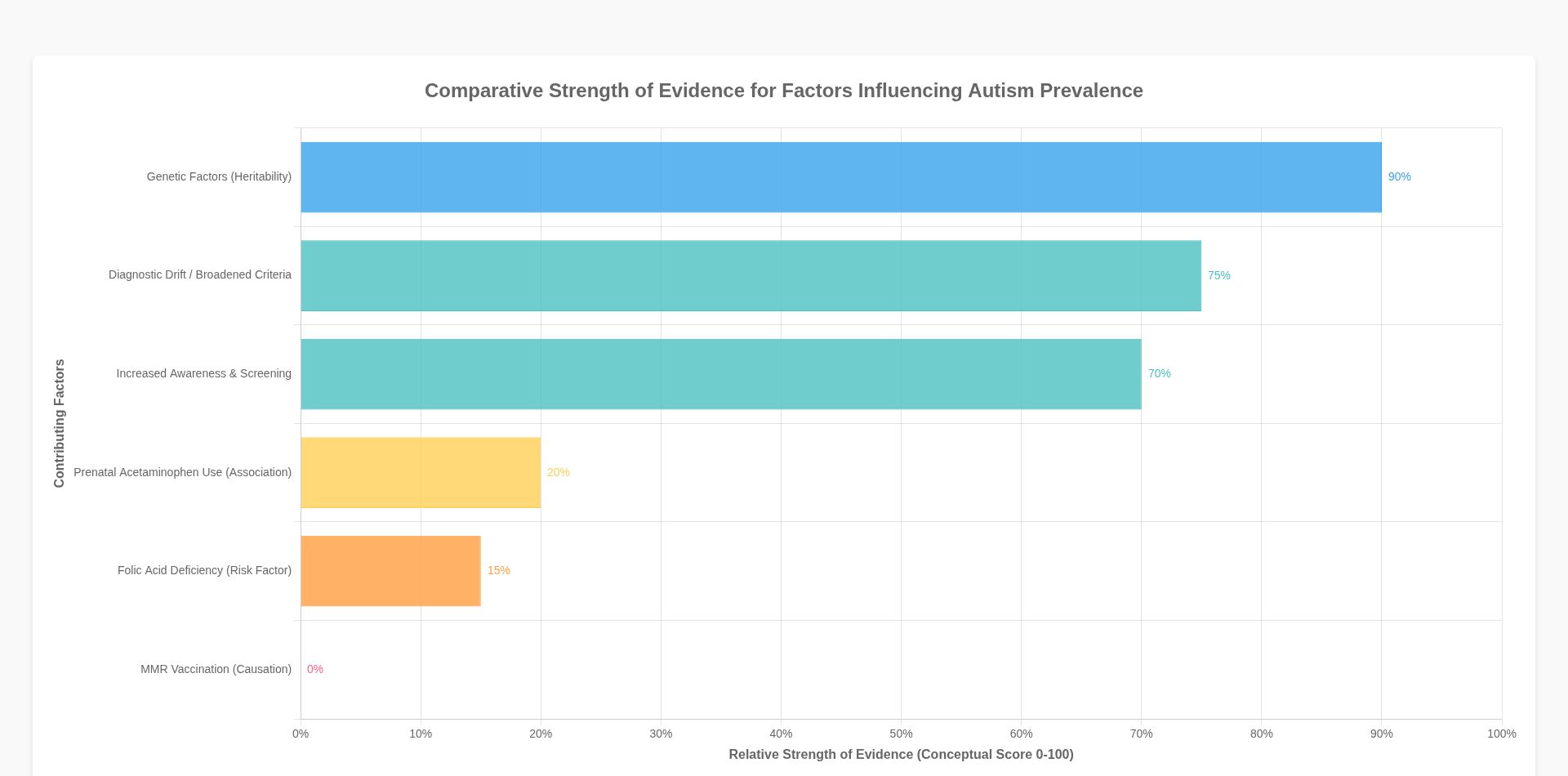
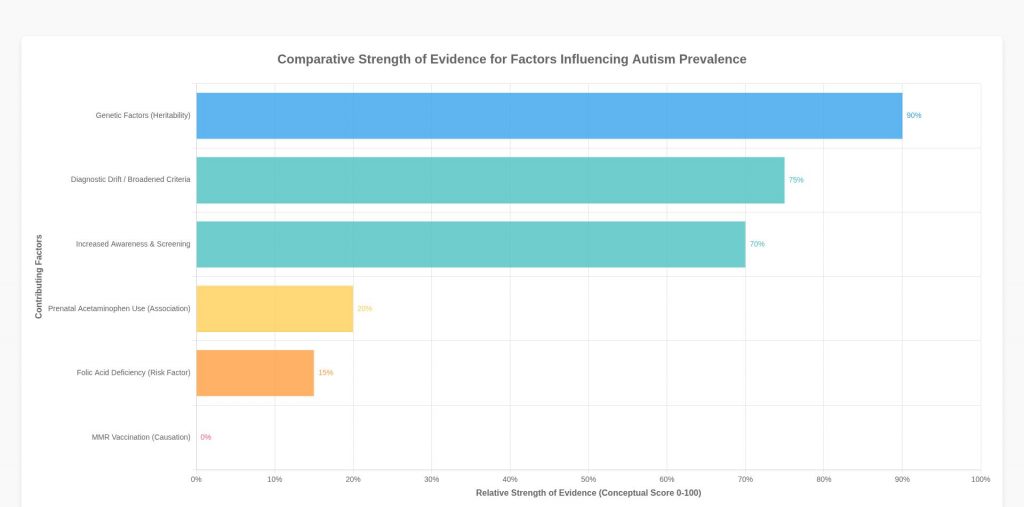
Two central claims address prenatal factors: the use of acetaminophen during pregnancy and folic acid deficiency as direct causes of autism. While these topics are areas of active research, presenting them as definitive causes is a misrepresentation of the current state of scientific knowledge, which points toward complex associations and risk factors rather than simple causal links.
1.1 The Acetaminophen (Tylenol) and Autism Link: Correlation vs. Causation
The assertion that acetaminophen use during pregnancy causes autism simplifies a complex and still-evolving body of research. Multiple epidemiological studies have investigated a potential association between prenatal acetaminophen exposure and neurodevelopmental outcomes, including ASD and Attention-Deficit/Hyperactivity Disorder (ADHD) . A 2021 meta-analysis of cohort studies involving over 132,000 mother-child pairs reported a 19% increased risk of ASD symptoms associated with prenatal acetaminophen exposure . Another 2024 study similarly noted a 19% increased risk for autism or ADHD symptoms in children with prenatal exposure .
However, these findings must be interpreted with significant caution. First, the observed risk increases are modest, and association does not equal causation. Researchers consistently highlight the challenge of controlling for confounding variables. For instance, the underlying maternal conditions necessitating acetaminophen use—such as fever, infection, inflammation, or chronic pain—may themselves be independent risk factors for adverse neurodevelopmental outcomes. The medication might be an indicator of an underlying issue rather than the causal agent itself.
Scientific literature emphasizes that while acetaminophen is generally considered relatively safe during pregnancy, more research is needed to fully understand its effects . Some studies propose plausible biological mechanisms for how acetaminophen might affect neurodevelopment, while others note the mother’s metabolism of the drug during pregnancy is particularly efficient, which could mitigate fetal exposure . The current scientific consensus does not support a definitive causal link. Major health organizations still view acetaminophen as a safer option for pain and fever management during pregnancy compared to alternatives like nonsteroidal anti-inflammatory drugs (NSAIDs). Advising a blanket avoidance of acetaminophen could lead pregnant individuals to endure untreated fever or pain, which carry their own established risks to the fetus, or to use medications with greater known risks. The claim overstates the certainty of the evidence and fails to convey the critical distinction between a statistical association and a proven causal relationship.
1.2 Folic Acid Deficiency: A Risk Factor, Not a Singular Cause
The claim that folic acid deficiency causes autism is another oversimplification. Unlike the acetaminophen hypothesis, the role of folic acid in neurodevelopment is well-established. Adequate maternal folate levels are crucial for preventing neural tube defects, and supplementation is a cornerstone of prenatal care. Research has extended this understanding to investigate its role in ASD. Several studies suggest that maternal folic acid supplementation, particularly in the periconceptional period, is associated with a reduced risk of ASD in offspring . A 2023 case-control study underscored the importance of prenatal care to ensure optimal supplementation and nutrition to mitigate ASD risk .
Therefore, folic acid deficiency can be accurately described as a modifiable risk factor for ASD, but it is not a singular cause. Autism is a complex neurodevelopmental condition with a strong genetic component, influenced by a combination of genetic and environmental factors . No single nutritional deficiency has been shown to cause autism in isolation. The HHS proposal to cover Leucovorin (a form of folinic acid) may be based on emerging research into cerebral folate deficiency, a rare condition sometimes associated with autism, but this is a specific metabolic issue affecting a small subset of the autistic population, not a universal cause. Promoting folic acid supplementation is a sound public health message, but framing its deficiency as a primary cause of the overall rise in autism prevalence is a misrepresentation of the multifactorial etiology of the disorder.
2. Examining Misconceptions About Prevalence and Diagnosis
Several of the alleged HHS claims dismiss established epidemiological explanations for the rising prevalence of ASD, instead relying on anecdotal evidence and flawed comparisons. These assertions include the idea that the Amish do not have autism and that diagnostic drift is not a valid explanation.
2.1 The Myth of the Autism-Free Community: The Case of the Amish
The claim that the Amish do not have autism is a persistent myth often used to suggest that a simpler, non-industrialized lifestyle—frequently linked anecdotally to lower vaccination rates—protects against the condition. This assertion is factually incorrect. Research on psychiatric disorders in different cultures has documented autism within Old Order Amish populations. A 2016 publication noted a 1% prevalence rate among the Old Order Amish, which is comparable to rates found in the general Western population at the time .
The perception that autism is rare or nonexistent in such communities is more likely a result of cultural, social, and diagnostic factors. Insular communities like the Amish may have different systems of social support, varying levels of engagement with mainstream medical and psychiatric services, and cultural interpretations of developmental differences that can lead to underdiagnosis or a lack of formal reporting. While studies have noted differences in the incidence of certain conditions like asthma in Amish communities, these are often linked to specific environmental exposures (like microbial diversity) and cannot be generalized to complex neurodevelopmental conditions . Using the Amish as “proof” against modern environmental causes of autism is a form of ecological fallacy that ignores both evidence of autism’s existence in the community and the numerous confounding variables that differentiate their lifestyle from the general population.
2.2 Diagnostic Drift: A Core Component of Increased Prevalence
The dismissal of “diagnostic drift” as a primary driver of the autism “epidemic” contradicts a vast body of epidemiological evidence. Diagnostic drift, also known as diagnostic substitution or changing diagnostic criteria, is a critical factor in explaining the observed increase in prevalence over the past three decades . This phenomenon encompasses several related elements:
- Broadening Diagnostic Criteria: The criteria for diagnosing autism have expanded significantly since the 1980s. The introduction of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) in 1994 included Asperger’s Syndrome and Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS), bringing many individuals with milder presentations under the autism umbrella. The current DSM-5 (2013) further refined the diagnosis into a single “Autism Spectrum Disorder,” recognizing the wide range of presentations.
- Increased Awareness and Screening: Public and professional awareness of autism has skyrocketed. This has led to better and earlier screening by pediatricians, educators, and parents, identifying children who would have been missed in previous generations.
- Diagnostic Substitution: Many individuals who would have previously been diagnosed with other conditions, such as intellectual disability or language disorder, are now correctly identified as being on the autism spectrum. Research has shown that as autism diagnoses have increased, diagnoses of intellectual disability have decreased, suggesting a shift in diagnostic labeling rather than a true increase in the absolute number of neurodevelopmentally diverse children.
- Access to Services: An official autism diagnosis is often a prerequisite for accessing specialized educational and therapeutic services. This incentivizes parents and clinicians to seek a formal diagnosis, further contributing to the recorded prevalence rates.
The claim that the California M.I.N.D. Institute “debunked” diagnostic drift is a mischaracterization of research. While the exact contribution of diagnostic drift versus a true increase in incidence is debated, no credible scientific institution has dismissed its significant role. The argument that there “aren’t many old people with severe, head-banging-against-wall autism” is a flawed appeal to anecdote. In previous generations, such individuals were often institutionalized, misdiagnosed with conditions like childhood schizophrenia, or simply hidden from public view, making them invisible in population statistics and public memory. They existed, but the diagnostic label and societal response were different. To deny the role of diagnostic drift is to ignore the fundamental evolution of psychiatric nosology and public health practice .
3. The Enduring Vaccine-Autism Controversy
Despite being one of the most thoroughly debunked claims in modern medicine, the idea that vaccines, particularly the Measles, Mumps, and Rubella (MMR) vaccine, cause autism persists. The HHS’s alleged validation of this theory and its related claims represents a dangerous departure from established science and public health policy.
3.1 MMR Vaccination and Autism: A Discredited Hypothesis
The origin of the MMR-autism scare was a fraudulent 1998 paper by Andrew Wakefield, which was retracted in 2010 after investigations revealed ethical violations and data falsification . Since then, numerous large-scale, high-quality epidemiological studies conducted across the globe, involving millions of children, have consistently found no causal link between the MMR vaccine and autism . The Institute of Medicine (now the National Academy of Medicine) has also discredited any link between the two . The scientific community considers the case closed: vaccines do not cause autism .
Giving credence to mothers who are sure their children’s autism resulted from “vaccine injuries” is an example of prioritizing anecdote over robust scientific evidence. While parental observations are invaluable for understanding a child’s developmental history, the temporal association between vaccination (which occurs during early childhood) and the emergence of noticeable autistic traits (which also become apparent in early childhood) often leads to a logical fallacy known as post hoc ergo propter hoc (“after this, therefore because of this”). The timing is coincidental, not causal. Validating this misinformation undermines public trust in life-saving vaccination programs and diverts attention from genuine research into the complex genetic and environmental factors that do contribute to autism .
3.2 Splitting Vaccines: Medically Unsound and Riskier
The suggestion that splitting the MMR vaccine into separate components would be “safer” and result in a lower total dosage is scientifically unfounded. This idea stems from the discredited notion that the combined vaccine overwhelms the immune system. In reality, a child’s immune system successfully handles thousands of antigens every day from their environment. The number of antigens in the entire childhood vaccination schedule is minuscule by comparison.
Furthermore, a separated vaccine schedule offers no safety benefits and introduces significant risks:
- Delayed Protection: Spacing out the vaccines leaves children vulnerable to measles, mumps, and rubella for longer periods. Measles, in particular, is a highly contagious and dangerous disease that can lead to pneumonia, encephalitis, and death.
- Increased Injections: A separated schedule requires more visits to the doctor and more injections, which can be traumatic for children and pose a greater logistical burden on families.
- No Reduction in “Dosage”: The amount of viral antigen in the combined vaccine is carefully calibrated to be effective. Splitting it does not reduce the total amount needed for immunity; it simply spreads it out over time.
The recommendation to split the MMR vaccine is not based on any immunological or pediatric evidence. It is a misguided attempt to appease vaccine hesitancy that ultimately compromises child health and public safety.
4. Flawed International Comparisons and Unsubstantiated Claims
The final set of claims relies on simplistic and misleading international comparisons and broad, unsupported statements to bolster its arguments. These assertions fail to withstand even basic scientific scrutiny.
4.1 The Case of Cuba: An Ecological Fallacy
The claim that “Cuba doesn’t use Tylenol and they have low autism rates” is a textbook example of the ecological fallacy. This line of reasoning incorrectly assumes that a country-level correlation (or lack thereof) can be used to make inferences about individual risk. There are countless differences between Cuba and other nations that could explain variations in reported autism prevalence, including:
- Genetics: The genetic makeup of the Cuban population is different.
- Environment: Diet, pollution levels, and exposure to infectious diseases vary significantly.
- Healthcare System: Diagnostic practices, access to specialists, and public health surveillance systems are not directly comparable .
- Cultural Norms: Cultural understanding and reporting of developmental disorders can differ dramatically.
Global estimates of ASD prevalence vary, with American and European countries often reporting higher rates (around 1%) compared to other regions . This is widely believed to reflect differences in diagnostic infrastructure and awareness rather than a true difference in incidence. There is limited robust, publicly available data on autism prevalence in Cuba, making any direct comparison highly speculative. While some research has been conducted with Cuban communities, such as studies on parental perspectives, these do not provide the epidemiological data needed to make such a sweeping claim . Attributing a hypothetical lower rate to the absence of a single common medication is a gross oversimplification that ignores dozens of more plausible confounding factors.
4.2 “No Stone Unturned”: A False Assertion
The declaration that HHS “left no stone unturned” is demonstrably false. A thorough investigation would have engaged with the vast scientific literature that refutes these claims. It would have consulted with leading epidemiologists, geneticists, pediatricians, and autism researchers who have dedicated their careers to understanding this complex condition. A genuine inquiry would have prioritized systematic reviews and meta-analyses over isolated studies, anecdotes, and debunked theories. Instead, the claims suggest a process of confirmation bias, where conclusions were formed first, and supporting “evidence”—however weak—was sought afterward. This approach is the antithesis of the scientific method and is profoundly damaging to public health and public trust.
5. Conclusion and Recommendations
The claims analyzed in this paper represent a significant departure from medical and scientific consensus on the causes and epidemiology of Autism Spectrum Disorder. By promoting theories based on weak associations, debunked hypotheses, and flawed reasoning, such public pronouncements risk causing tangible harm. They may lead pregnant individuals to make unsafe health choices, erode trust in essential public health measures like vaccination, and misdirect valuable resources away from evidence-based research and support services for autistic individuals and their families.
A responsible public health approach must be grounded in scientific rigor and transparent communication. The following recommendations are offered for policymakers, healthcare professionals, and researchers to foster a more accurate and productive public discourse on autism.
For Policymakers and Public Health Agencies:
- Promote Evidence-Based Communication: Public health messaging must clearly distinguish between association and causation. Information released to the public should be based on the totality of evidence from systematic reviews and meta-analyses, not on isolated or preliminary studies.
- Combat Misinformation: Actively debunk persistent myths, particularly regarding vaccines, with clear, accessible, and consistent messaging across all platforms. Partner with community leaders and trusted medical professionals to disseminate accurate information.
- Fund Unbiased Research: Direct research funding toward promising areas, including the complex interplay of genetics and environmental risk factors, early biomarkers, and the development of effective, individualized supports and therapies.
- Support Autistic Individuals and Families: Shift the focus from a singular search for a “cure” or a cause to blame, towards improving the quality of life for autistic individuals. This includes funding for diagnostic services, early intervention, inclusive education, and adult support programs.
For Healthcare Professionals:
- Provide Accurate Patient Counseling: Clinicians should be prepared to discuss parental concerns about autism causes with empathy, while providing clear, evidence-based information regarding topics like prenatal medication use and vaccination.
- Stay Informed on Current Research: Continuously update knowledge on ASD etiology and epidemiology to provide the most accurate guidance to patients and their families.
- Advocate for Public Health: Use their trusted position in the community to advocate for evidence-based policies and to counter health misinformation.
For the Research Community:
- Improve Research Communication: Researchers must work to make their findings more accessible to the public and policymakers, providing context and clearly explaining the limitations of their work to prevent misinterpretation.
- Focus on Multifactorial Models: Continue to investigate the complex gene-environment interactions that contribute to autism, moving beyond the search for single, simplistic causes.
- Involve the Autism Community: Engage autistic individuals and their families in setting research priorities to ensure that scientific efforts align with the practical needs and lived experiences of the community .
In summary, understanding the rise in autism prevalence requires a nuanced appreciation of genetics, evolving diagnostic practices, and genuine environmental risk factors—not the pursuit of simplistic and unsupported theories. By adhering to the principles of evidence-based medicine and public health, we can move beyond damaging speculation and toward a future that better supports the well-being of all autistic individuals.
References
General
[1] Acetaminophen in pregnancy and attention-deficit and hyperactivity disorder and autism spectrum disorder. https://journals.lww.com/greenjournal/fulltext/2025/02000/aspx
[2] Acetaminophen use during pregnancy and children’s risk of autism, ADHD, and intellectual disability. Jama. https://jamanetwork.com/journals/jama/article-abstract/2817406
[3] Prenatal and postnatal exposure to acetaminophen in relation to autism spectrum and attention-deficit and hyperactivity symptoms in childhood: Meta-analysis …. https://link.springer.com/article/10.1007/s106Fmemberid%3Fmemberid
[4] Evaluating the role of susceptibility inducing cofactors and of acetaminophen in the etiology of autism spectrum disorder. Life. https://pmc.ncbi.nlm.nih.gov/articles/PMC11355895/
[5] The dangers of acetaminophen for neurodevelopment outweigh scant evidence for long-term benefits. Children. https://www.mdpi.com/2227-9067/11/1/44
[6] Acetaminophen causes neurodevelopmental injury in susceptible babies and children: No valid rationale for controversy. https://pmc.ncbi.nlm.nih.gov/articles/PMC10915458/
[7] … DISORDER-THE POSSIBLE TRIGGER OF PHARMACOLOGICAL INTERVENTIONS USED IN INFERTILITY TREATMENTS OR DURING PREGNANCY… https://farmaciajournal.com/wp-content/uploads/art-01-Varlas_Penes_Zetu_1109-1119.pdf
[8] Association of NSAIDs and Acetaminophen Prescriptions During Pregnancy With Autism Spectrum Disorders in the Child. search.proquest.com. https://search.proquest.com/openview/5a3f75478525e1a09eed02beb557629d/1?pq-origsite=gscholar&cbl=18750&diss=y
[9] Maternal Folate Status and Risk Factors for Autism Spectrum Disorders. search.proquest.com. https://search.proquest.com/openview/1e930f5bba5a8750&diss=y
[10] Autism spectrum disorder. https://www.ijpp.in/admin/uploadimage/Vol.26_No.2.pdf#page=5
[11] Do psychiatric disorders differ in different cultures?. https://api.taylorfrancis.com/content/chapters/edit/download?identifierNameterpdf
[12] Public Health struggles to square hygiene with diversity: research on the link between microbiomes and immune function puts the “hygiene hypothesis” to rest. EMBO reports. https://www.embopress.org/doi/abs/10.15252/embr.202051540
[13] Autism Causes, Prevention and Treatment: Vitamin D Deficiency and the Explosive Rise of Autism Spectrum Disorder. books.google.com. https://books.google.com/books?hl=en&lr=&id=yALS8Oi8
[14] Autism Spectrum Disorder: Bioregenerative Medicine With Stem Cell Therapy. books.google.com. https://books.google.com/booLXvOMvs
[15] … evidence that certain heavy metals, toxic organic chemicals and infectious agents play an important role in triggering autism and other environmental health problems …. https://ijvtpr.com/index.php/IJVTPR/article/view/4
[16] Moving past the vaccine/autism controversy-to examine potential vaccine neurological harms. https://journals.sagepub.com/doi/abs/10.3233/JRS-200052
[17] The myth of vaccination and autism spectrum. https://www.sciencedirect.com/science/article/pii/S1090379821002312
[18] A case study of MMR vaccine skeptics. Recover Argum. https://books.google.com/books?hl=en&lr=&id=rfl0DwAAQBAJ&oi=fnd&pg=PT91&dq=MMR+vaccine+autism+debunked+studies,+California+MIND+Institute+diagnostic+drift,+autism+diagnostic+criteria+changes&ots=l4qcZFvxW3&sig=_-4EnZhKjJOTUZVtLJ1AmJyg3Dg
[19] Anti/Vax: Reframing the vaccination controversy. books.google.com. https://books.google.com/books?hl=en&lr=&id=4q94DwAAQBAJ&oi=fnd&pg=PR7&dq=MMR+vaccine+autism+debunked+studies,+California+MIND+Institute+diagnostic+drift,+autism+diagnostic+criteria+changes&ots=kqEp2stkkP&sig=HwUJpzePdTciCqjiqAWnZl0LYss
[20] Stop Autism Now!: A Parent’s Guide to Preventing and Reversing Autism Spectrum Disorders. books.google.com. https://books.google.com/books?hl=en&lr=&id=t4swDwAAQBAJ&oi=fnd&pg=PA5&dq=MMR+vaccine+autism+debunked+studies,+California+MIND+Institute+diagnostic+drift,+autism+diagnostic+criteria+changes&ots=DhMjSp1Yd4&sig=ENgVy-ZuAMmMXq_VHU4VoUAEg3Q
[21] Foolproof: Why misinformation infects our minds and how to build immunity. books.google.com. https://books.google.com/books?hl=en&lr=&id=LN1wEAAAQBAJ&oi=fnd&pg=PT5&dq=MMR+vaccine+autism+debunked+studies,+California+MIND+Institute+diagnostic+drift,+autism+diagnostic+criteria+changes&ots=hIx7D4xGOl&sig=0LtLT-zM6qCHtsJsPMP8vWr5GfM
[22] The Prevalence and incidence of congenital phenylketonuria in 59 countries: A systematic review. https://jpr.mazums.ac.ir/browse.php?a_id=352&slc_lang=en&sid=1&ftxt=1&html=1
[23] Biochemical, genetic and clinical diagnostic approaches to autism-associated inherited metabolic disorders. Genes. https://www.mdpi.com/2073-4425/14/4/803